Functional Endoscopic Sinus Surgery Versus Balloon Sinuplasty: Which One is Right for You?
Functional Endoscopic Sinus Surgery: Sinusitis, infection and/or inflammation of the sinus cavities, impacts the lives of approximately 37 million people in the US each year leading to $6 billion in annual healthcare expenses. The underlying causes of sinusitis include nasal allergies (often to pollens, molds, and pet dander), viral, bacterial, or fungal-related infections, and less commonly facial trauma, altered sinus/nasal anatomy, or impaired immune system. Acute bacterial infection often follows a viral upper respiratory infection, causing symptoms to relapse worse than before just when they seemed to be improving. While acute sinusitis lasts for up to 4 weeks and generally resolves spontaneously or with the help of antibiotics, the treatment of chronic sinusitis requires prolonged medical therapy with 2 or more weeks of antibiotics and often anti-inflammatory medications such as oral steroids and/or nasal steroid sprays. Allergy testing and allergy shots may also be required in patients with identifiable allergy triggers. Symptoms of sinusitis can dramatically impact quality of life, and may include facial pressure/pain, headaches, discolored nasal drainage, nasal congestion or blockage, and less common signs such as fever, loss of smell, and nosebleeds. When these symptoms occur frequently (4 or more times) throughout the year,or fail to improve with adequate medical therapy, then surgical intervention is indicated to provide lasting relief.

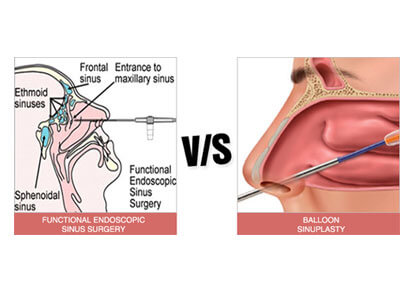
The purpose of this post is to compare the nature, indications, benefits, and risks of traditional functional endoscopic sinus surgery (FESS) with those of balloon sinuplasty so that patients suffering with sinusitis are prepared to make an informed decision regarding their selection of therapy.
Functional Endoscopic Sinus Surgery (FESS)
In traditional endoscopic sinus surgery, scopes and instruments are passed into the nostrils under general anesthesia and tissue is removed from the nasal cavities and sinus openings in order to clean out the sinuses, send cultures of infected secretions when encountered (which helps guide successful antibiotic therapy), correct a deviated septum and/or enlarged turbinates in order to relieve nasal congestion, and create windows into the sinuses that remain open, prevent sinus pressure/pain, allow for treatment of the sinuses with topical rinses during future flare-ups (such as antibiotic and steroid rinses, which avoid pills with multiple side effects), and allow for monitoring and clean out of the sinuses in the clinic setting in patients with ongoing inflammatory conditions (such as severe nasal allergies).
FESS is indicated for patients with unusual nasal anatomy that prohibits the use of balloon sinuplas ty, patients who have failed previous sinus surgery or balloon sinuplasty, patients with chronic inflammatory conditions (such as allergic fungal sinusitis or patients with extensive nasal polyps) that will necessitate ongoing access to the sinuses for medicated rinses, in-office removal of debris, and removal of recurrent polyps, and for any patient with a history of complicated sinusitis (infection that has eroded through bone and extends into the orbit, the cranium, or the soft tissues of the forehead). Other findings on a patient’s CT scan may also suggest the need for FESS rather than a balloon procedure, including ingrowth of new bone that requires removal, soft tissue masses concerning for tumors or extensive polyps, and bony defects of the base of the skull that place patients at increased risk for leakage of cerebrospinal fluid and meningitis.
The major benefits of FESS over balloon sinuplasty are that it has been a reliable treatment for sinusitis since the 1980’s with long-lasting improvements in symptoms (greater than 10 years in major studies of FESS), it allows for more extensive removal of tissues and a complete septoplasty to provide maximal relief of nasal congestion and sinus blockages, it allows for in-office management of most future sinus-related problems, and it allows for future treatment of sinusitis with medicated rinses that may avoid the use of pills with many side effects as previously discussed. These benefits must be weighed, however, against the increased risks of removing significant amounts of tissue from the inside of the nose and sinuses. Bleeding during surgery, while normally not extensive, can be more significant in FESS than in balloon sinuplasty. Post-operative recovery time is generally one to two weeks, with limited activity during that period. Post-operative nasal crusting, infections, and nosebleeds are the most common minor side effects of FESS. Major complications are very rare in experienced hands, the most common being significant bleeding requiring a nasal pack or cauterization under anesthesia, numbness of the upper dentition that may be permanent, scarring within the nose that causes symptoms and necessitates additional surgery, and impaired healing of the sinuses causing chronic post-operative infections.
Balloon Sinuplasty
In balloon sinuplasty scopes and instruments are placed through the nostrils while awake under local anesthesia or under light intravenous sedation (usually in the clinic setting), and a balloon is passed over a wire and into the sinus openings. The balloon is inflated to dilate the natural drainage pathways of each sinus, which are improved permanently as thin bones are broken and remodeled during this process. The sinuses are washed through the balloon catheter, and cultures can be sent if infected secretions are encountered. The mucosal lining of the sinus openings is preserved, as the balloon is less traumatic than traditional FESS. Additional procedures might be added to address limited deformities of the nasal septum and shrink the turbinates with needle ablation procedures. Some tissue removal is often performed to open the anterior ethmoid cells and create a wider drainage pathway for the major ity of the sinuses.
Balloon sinuplasty is indicated for patients with recurrent acute sinusitis (4 or more episodes of acute sinus infections per year) and mild chronic sinusitis without extensive nasal polyps. Other contraindications to balloon procedures were already mentioned, and imply altered anatomy that would prohibit balloon dilation or moderate to severe disease that requires more extensive tissue removal. Indications for balloon sinuplasty are similar to FESS, and the decision to proceed with one versus the other must reflect the underlying cause of each patient’s sinusitis and the long-term goals of therapy.
The major benefits of balloon sinoplasty over FESS include a faster and less bothersome recovery period (patients are often able to return to work the next day, and activity limitations depend upon the extent of additional interventions such as septoplasty), and significantly less risk for major complications. Most patients report very little discomfort following balloon sinuplasty, and crusting, bleeding, and post-operative infection are less common than following FESS. Major complications are exceedingly rare in balloon sinuplasty. The efficacy, or success rate, of the procedure has been shown in studies to equal outcomes from FESS during the initial 2 to 5 years after the procedure when performed in APPROPRIATELY SELECTED patients. Additional studies are underway to determine how well balloon sinuplasty improves symptoms beyond 5 years. Many patients who fail to improve following balloon sinuplasty are offered the procedure despite being less-than-ideal candidates.
Deciding Which Procedure Best Meets Your Needs and Treatment Goals
Both FESS and balloon sinuplasty are considered safe and effective surgical interventions in the treatment of sinusitis. The underlying cause of sinusitis is the most important factor to consider in deciding between the two, when both are seemingly good options. Patients with recurrent acute sinusitis or frequent facial pressure/pain may have sinus openings that are narrow and at risk for obstructing with any inciting factor such as a common cold. In the absence of this inciting factor, they likely have normal sinuses with adequate function to prevent chronic infections. Balloon sinuplasty is often the ideal solution for these patients, as the sinus openings are dilated to prevent recurrence of symptoms without disturbing the natural function of the sinus. Patients with mild chronic sinusitis may also see resolution of their symptoms with balloon dilation to improve drainage of the sinuses and wash away any pathogens causing their chronic symptoms. Appropriately selected balloon sinuplasty patients can expect treatment results equivalent to FESS without the discomfort and risks involved with extensive tissue removal.
On the contrary, patients with chronic inflammatory conditions that cannot be adequately, consistently, or safely controlled with oral medications long-term will substantially benefit from FESS, and the ability to apply topical medicated rinses through surgical sinus windows and have their sinuses monitored and managed through these windows in the clinic setting for as long as their condition persists (often for life) should be their primary goal in selecting a surgical treatment. Chronic inflammatory conditions do not resolve with surgical therapy alone. The purpose of surgery in this setting is to improve symptoms AND the long-term ability to manage the condition through wide-open sinuses, which is not feasible with balloon dilation alone. Examples of chronic inflammatory conditions include: allergic fungal sinusitis with thick, sticky mucous that fails to drain on its own, Samter’s triad (asthma, nasal polyps, and aspirin sensitivity), chronic sinusitis with extensive nasal polyps (which are a result of inflammation), chronic sinusitis caused by moderate to severe inhalant allergies (molds, pollens, pet dander, etc.) that cannot be avoided and fail to respond to medical management alone, and chronic sinusitis secondary to Afrin (nasal decongestant spray) abuse leading to chronically inflamed and swollen tissues throughout the nasal cavities.
Need More Information?
If you or someone you know in Houston suffers from sinusitis-related symptoms that are impacting quality of life, please call (713) 791-0700 or visit us online at www.houstonadvancedsinus.com to schedule a consultation with Houston’s premier fellowship-trained sinus specialist. The Rhinologists at Houston Advanced Nose and Sinus offer the full range of sinus treatments, and will ensure that patients receive the best possible care.

